Treating the Root Cause
,
This is a placeholder for the Yext Knolwedge Tags. This message will not appear on the live site, but only within the editor. The Yext Knowledge Tags are successfully installed and will be added to the website.
Blog Layout
Menopause: Functional & Holistic Treatments
Dr. Erin Thorne
Managing Menopause Holistically
For the vibrant women of Seattle, embracing life's changes often includes navigating the transformative journey of menopause. This natural phase in a woman's life can bring with it a spectrum of symptoms that impact physical and emotional well-being. While some women opt for Hormone Replacement Therapy (HRT), others seek holistic solutions to manage menopause symptoms, including weight gain. In this blog, we'll explore how Seattle women can empower themselves through holistic approaches to menopause, weight management, HRT, and symptom relief.
Understanding Menopause and Its Impact
Menopause typically occurs in women between their late 40s and early 50s. This significant life transition is characterized by the cessation of the menstrual cycle and a decline in hormone production, particularly estrogen and progesterone. These hormonal changes can lead to a variety of symptoms, including hot flashes, mood swings, insomnia, and weight gain.
Hormone Replacement Therapy (HRT) in Seattle
Hormone Replacement Therapy (HRT) is a conventional medical approach to manage menopausal symptoms. It involves replacing the hormones (usually estrogen and sometimes progesterone) that decrease during menopause. While HRT can be effective in alleviating many menopausal symptoms, it's not without potential risks, and it may not be suitable for all women. Consulting with a healthcare provider is crucial when considering HRT.
Holistic Approaches for Seattle Women
Seattle is known for its holistic and health-conscious culture, making it an ideal place for women to explore alternative approaches to menopause. Here are holistic strategies that can complement or even replace traditional HRT:
- Nutrition and Diet:
Seattle's abundance of fresh, organic produce makes it easy for women to maintain a balanced diet rich in whole foods, fruits, vegetables, and lean proteins. Incorporating soy, flaxseeds, and foods high in calcium and vitamin D can be particularly helpful during menopause.
- Active Lifestyle:
Seattle's natural beauty encourages an active lifestyle. Regular physical activity, such as hiking, biking, or even mindful walks in local parks, can help manage weight and improve overall well-being.
- Mindfulness Practices:
Seattle women can embrace mindfulness practices like yoga, meditation, and tai chi to reduce stress, enhance mood, and find inner peace during the ups and downs of menopause.
- Natural Supplements:
Herbal supplements like black cohosh, evening primrose oil, and red clover are popular among Seattle women seeking relief from menopausal symptoms. Always consult with a healthcare provider before adding supplements to your routine.
- Acupuncture:
Seattle offers a thriving acupuncture community. Many women find this traditional Chinese medicine practice to be effective in reducing hot flashes, improving sleep, and restoring balance during menopause.
- Stress Management:
Seattle's focus on well-being includes various stress-management resources, such as mindfulness workshops, therapy, and support groups. Reducing stress is essential for managing menopause symptoms.
Managing Weight During Menopause in Seattle
Seattle's love for outdoor activities and farm-to-table cuisine can make weight management during menopause a positive experience. Here are some tips for maintaining a healthy weight:
- Local, Fresh Foods:
Embrace the bountiful local produce and seafood to create nutritious and delicious meals that support weight management.
- Community Fitness:
Participate in group fitness classes, join hiking groups, or take up water sports like kayaking or paddleboarding to stay active while connecting with like-minded women.
- Farmers' Markets:
Explore the numerous farmers' markets in Seattle to find fresh, organic, and locally sourced ingredients for your meals.
- Mindful Eating:
Savor every bite and eat with intention. Seattle's focus on conscious living can extend to mindful eating practices.
Seattle women approaching or experiencing menopause have a wealth of holistic resources at their disposal. While HRT is a viable option, embracing the city's health-conscious culture allows women to explore alternative approaches to managing menopause symptoms, maintaining a healthy weight, and finding balance during this transformative phase. Remember to consult with a healthcare provider to tailor a holistic approach that aligns with your individual needs and preferences. In Seattle, the journey through menopause can be an empowering and transformative experience.
By Dr. Erin Thorne, ND
•
June 23, 2024
Managing ADHD holistically involves understanding how various factors, including hormonal changes during menopause and conditions like PCOS, affect focus and attention. Let’s explore the connections between ADHD and these factors, and discuss strategies to manage ADHD through lifestyle, nutrition, and other holistic approaches. ADHD and Hormonal Changes Impact of Low Estrogen Estrogen plays a significant role in cognitive function. During menopause and in conditions like PCOS, low estrogen levels can exacerbate ADHD symptoms by impairing focus and attention. • Focus and Attention: Estrogen helps regulate neurotransmitters like dopamine and serotonin, which are crucial for attention and mood. Lower estrogen levels can lead to decreased dopamine activity, impacting your ability to focus. Sleep and ADHD Importance of Sleep Quality sleep is essential for managing ADHD. Sleep disturbances can worsen ADHD symptoms by affecting cognitive functions and emotional regulation. • Sleep Guidelines: Aim for 7-9 hours of quality sleep per night. Establish a regular sleep routine, create a calming bedtime environment, and avoid stimulants like caffeine close to bedtime. Exercise and ADHD Exercise Benefits Regular physical activity can significantly improve ADHD symptoms by increasing dopamine and norepinephrine levels, which help with attention and mood regulation. • Exercise Routine: Incorporate both aerobic exercises (like running or cycling) and strength training into your routine. Aim for at least 150 minutes of moderate-intensity exercise per week. Stress and ADHD Managing Stress Stress can exacerbate ADHD symptoms by increasing cortisol levels, which interfere with cognitive functions and emotional stability. • Stress Reduction: Practice mindfulness, yoga, or meditation to manage stress. Ensure you have time for relaxation and activities you enjoy. Multitasking and ADHD Avoiding Multitasking Multitasking can overwhelm the brain, making ADHD symptoms worse. Focus on one task at a time to improve productivity and reduce stress. Nutrition, Lifestyle, and Exercise for ADHD Nutrition Guidelines • Balanced Diet: Eat a diet rich in whole foods, including fruits, vegetables, lean proteins, and healthy fats. Avoid processed foods and high sugar intake. • Supplements: Consider omega-3 fatty acids, magnesium, zinc, and vitamin D to support brain health. Consult with a healthcare provider before starting any supplements. Lifestyle Tips • Routine and Structure: Establish a daily routine to create predictability and reduce anxiety. • Environment: Create a distraction-free environment for work and relaxation. Genetic Factors and ADHD MTHFR and Other Genetic Mutations Genetic mutations like MTHFR can impact neurotransmitter synthesis and methylation processes, influencing ADHD symptoms. Consider genetic testing and personalized interventions if you suspect genetic factors play a role. Medication for ADHD Benefits and Side Effects While medications like stimulants can be effective for managing ADHD, they come with potential side effects and long-term risks such as sleep disturbances, appetite suppression, and cardiovascular issues. • Medications: Discuss with your healthcare provider the risks and benefits of ADHD medications and explore alternative treatments if needed. Supplements and Nutrients for ADHD Key Supplements • Omega-3 Fatty Acids: Supports brain health and reduces inflammation. • Magnesium: Helps with relaxation and cognitive function. • Zinc and Iron: Important for neurotransmitter regulation. Dopamine and ADHD Dopamine’s Role Dopamine plays a critical role in attention and reward mechanisms. Both excessive and deficient dopamine activities can worsen ADHD symptoms. • Finding the Sweet Spot: Engage in activities that provide a balanced dopamine response, such as creative hobbies, exercise, and achievable goal-setting. Other Neurotransmitters • Serotonin and Norepinephrine: These neurotransmitters also impact ADHD symptoms. Balanced levels can improve mood and focus. Toxins and ADHD Avoiding Toxins • Red Food Coloring and Additives: These can exacerbate ADHD symptoms. Avoid processed foods with artificial additives. • Environmental Toxins: Minimize exposure to environmental toxins by choosing organic foods and using natural household products. Creating a Healthy Environment • Supportive Home Environment: Keep your living space organized and free from clutter. Use planners and reminders to stay on track. • Achieving Goals: Set and achieve small, manageable goals to boost confidence and motivation. Social Media and Multitasking Impact on ADHD Excessive use of social media and multitasking can worsen ADHD symptoms by overwhelming your attention span and increasing anxiety. • Limit Screen Time: Set boundaries for social media use and focus on single-tasking to improve concentration. Conclusion Holistically managing ADHD involves a multifaceted approach that addresses hormonal changes, sleep, exercise, nutrition, and lifestyle factors. By creating a supportive environment, prioritizing self-care, and understanding the role of neurotransmitters and genetics, you can effectively manage ADHD symptoms and improve your overall quality of life. Take care, and remember that small, consistent changes can make a big difference. Yours in health, Dr. Erin Thorne

By Dr. Erin Thorne, ND
•
June 23, 2024
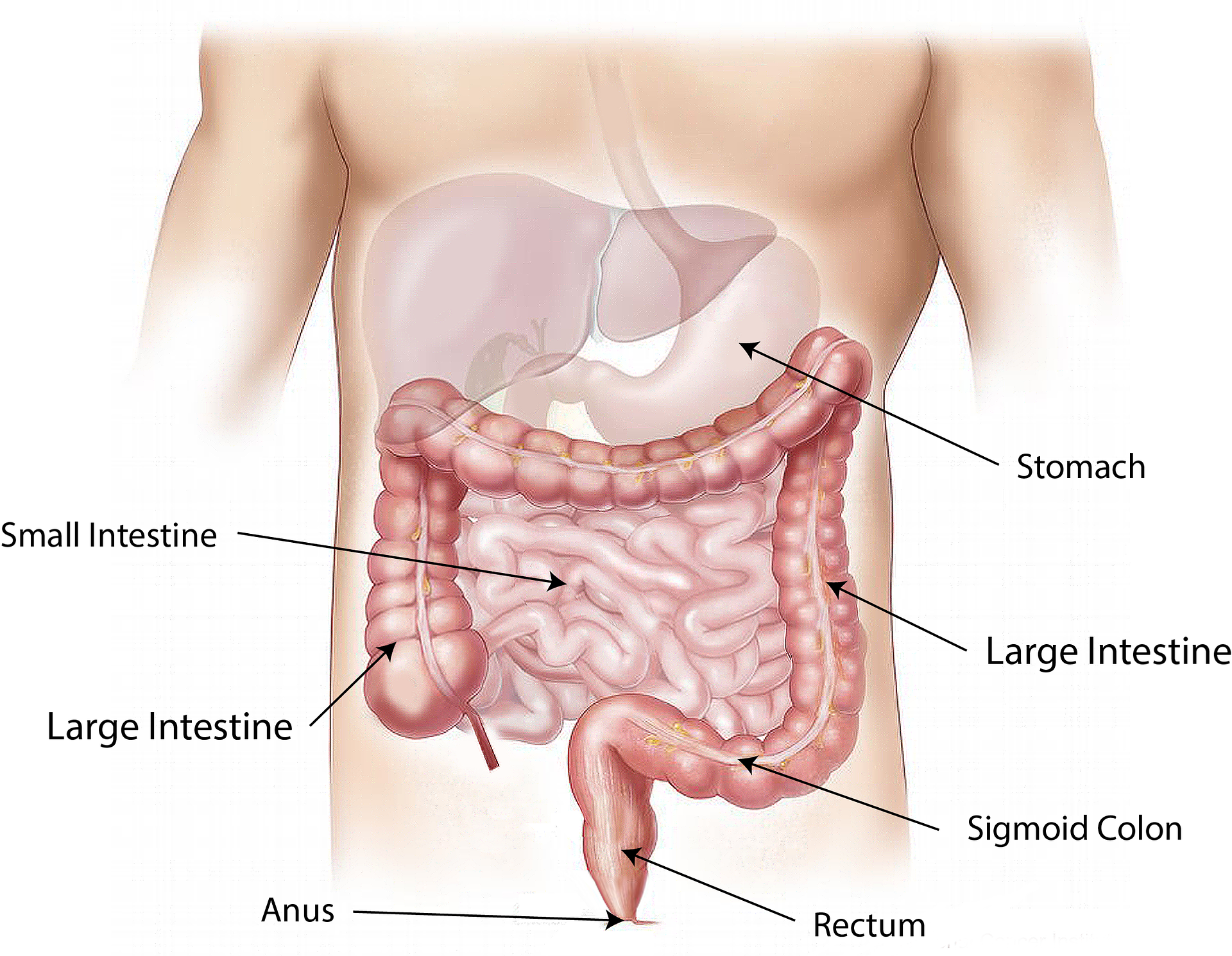
Navigating weight loss and maintaining your current weight during menopause can be challenging, but with the right approach, it’s absolutely achievable. As a naturopathic doctor and functional medicine provider who deeply understands the unique hormonal shifts during this stage, I’m here to guide you through a stepwise process that prioritizes overall well-being while focusing on weight loss. Let’s explore this journey together, emphasizing gut health, hormonal balance, exercise, nutrition, and mindfulness. Step 1: Heal Your Gut Gut Health: Begin by improving your gut health to enhance nutrient absorption, promote bacterial diversity, and reduce inflammation. This foundation is crucial for balancing hormones and supporting weight loss. Read My Article on Hormones and Estrogen/Microbiome. • Whole Foods: Focus on whole, unprocessed foods. Incorporate a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. • Soluble Fiber: Important for weight loss as it slows digestion, keeps you feeling fuller longer, and regulates blood sugar. Top 10 foods highest in soluble fiber include oats, apples, oranges, carrots, psyllium, flaxseeds, beans, lentils, barley, and Brussels sprouts. • Insoluble vs. Soluble Fiber: Insoluble fiber (found in whole grains and vegetables) aids in digestion and prevents constipation, while soluble fiber (found in oats and fruits) helps manage blood sugar levels and hunger. • Avoid: foods high in processed sugar and grains, food with pesticides, endocrine disruptors and microplasics. • POOP OFTEN to promote detoxification and off load all the inflammation in your gut. Inflammation contributes to stubborn weight by inhibiting proper insulin, hormone, thyroid and cortisol function. You should be pooping twice a day at least! I you're pooping only once or less a day this may be a reason to look into your guts impact on weight. Step 2: Address Stress and Cortisol Stress Management: Menopause can increase cortisol levels, leading to belly fat and weight gain. Implement stress-reducing activities: • Mindfulness and Meditation: Practice daily to reduce cortisol levels. I LOVE guided mediation on Insight Timer. My favorites are the ones from Sarah Blondin. • Yoga and Breathing Exercises: These can help manage stress and improve overall well-being. Square breathing, Box breathing, So-hum breathing • Testing cortisol with a 4-point cortisol curve to see if cortisol is impacting your weight loss journey. • Supplements and nutrients that support adrenals: adaptogens, magnesium, B6, cordyceps to name a few. Step 3: Prioritize Sleep Quality Sleep is: People who have poor sleep eat an average of 600 additional calories the next day to make up for the perceived deficit in energy the body requires. Poor sleep leads to overeating or poor food choices, less energy to prepare healthy meals and make healthy choices. Essential for cellular repair, removes inflammation and restocks the shelves for tomorrow Essential for Detox and removal of cellular waste Essential for hormonal balance, cortisol is your daytime hormone and melatonin is your nighttime hormone and both impact your ovary and thyroid hormones. Aim for 7-9 hours per night. ( I've been leaning more towards 9 lately!) • Sleep Hygiene: Establish a regular sleep schedule, create a restful environment, and avoid screens before bedtime. Step 4: Exercise Smartly Weight Lifting and High-Intensity Exercise: Building muscle improves insulin sensitivity and fat burn. Include: • Strength Training: At least 2-3 times a week. • High-Intensity Interval Training (HIIT): Effective for burning fat and boosting metabolism. Cardio for Heart Health and Stamina: • Dancing: An excellent form of cardio that’s fun and effective. ( my personal favorite!) • Walking, Running, Cycling: Regular cardio exercises that improve heart health. Step 5: Nourish Your Body Eating Before and After Exercise: Proper nutrition fuels your workouts and aids recovery. Don’t under-eat; your body needs energy! You should be eating within 30 minutes after a hard work out and always eat a protein carb fuel prior to workout. You don't want to run on cortisol, you need to run on fuel! • Balanced Meals: Include a mix of protein, carbs, and fats. • Cruciferous Vegetables: Broccoli, cauliflower, and kale help balance hormones. Calorie and Macro Tracking: • Calorie Tracking: Ensures you’re not overeating or undereating. • Macronutrient Calculations: Balance protein, carbs, and fats for optimal health. • Micronutrients: Ensure adequate intake of vitamins and minerals like calcium, magnesium, and vitamin D. Step 6: Set Mindful Goals Vision Board and Future Planning: • Set Goals: What do you want to achieve in the next 5, 10, 20 years? • Visualization: Create a vision board to keep you motivated. Step 7: Overcome Obstacles Managing Challenges: Acknowledge common obstacles like burnout, lack of time, frustration, and lack of results. Here’s how to stay on track: • Refocus and Stay Positive: Remember why you started and celebrate small victories. • Menopause Buddy and Community: Find support and encouragement from others on the same journey. Enjoy the Journey! You're more than that number on the scale! take breaks. Remeber that weight loss is a journey, you will lose weight and then plateau while your body adjusts. Focus on the Process: Rather than fixating on the scale, enjoy the journey. Celebrate improvements in your strength, stamina, and overall health. By prioritizing gut health, managing stress, ensuring quality sleep, engaging in smart exercise, nourishing your body, and setting mindful goals, you can successfully navigate weight loss during menopause. Remember, this journey is about improving your health and well-being, not just the number on the scale. Take care, and embrace the journey! Yours in health, Dr. Erin Thorne
By Dr. Erin Thorne, ND
•
June 23, 2024
As a naturopathic doctor and functional medicine provider, I want to address a condition that can significantly impact your digestive health and overall well-being: Small Intestinal Bacterial Overgrowth (SIBO) and Small Intestinal Fungal Overgrowth (SIFO). Understanding these conditions, their symptoms, causes, and treatments can help you manage and improve your gut health effectively. What is SIBO and SIFO? SIBO occurs when there is an abnormal increase in the number of bacteria in the small intestine, particularly types of bacteria not commonly found in that part of the digestive tract. SIFO, on the other hand, refers to an overgrowth of fungi in the small intestine. Both conditions can disrupt digestion and nutrient absorption, leading to a range of symptoms. Types of SIBO and SIFO SIBO is typically classified based on the predominant type of gas produced by the bacterial overgrowth: 1. Hydrogen-predominant SIBO: Often associated with diarrhea. 2. Methane-predominant SIBO: Often associated with constipation. 3. Hydrogen sulfide-predominant SIBO: Less common, but can cause symptoms like diarrhea and bloating. SIFO involves an overgrowth of fungi such as Candida, leading to similar digestive issues. Symptoms of SIBO and SIFO Here are ten common symptoms: 1. Bloating 2. Diarrhea 3. Constipation 4. Abdominal pain or discomfort 5. Excessive gas 6. Fatigue 7. Nausea 8. Unintended weight loss 9. Nutrient deficiencies (e.g., B12, iron) 10. Joint pain or aches Causes of SIBO and SIFO Ten common causes include: 1. Poor gut motility: Slow movement of food and waste through the digestive tract. 2. Low stomach acid: Reduces the ability to kill harmful bacteria. 3. Chronic stress: Affects gut function and immunity. 4. Antibiotic use: Disrupts normal gut flora. 5. Diet high in refined carbohydrates: Feeds harmful bacteria and fungi. 6. Irritable Bowel Syndrome (IBS): Often coexists with SIBO. 7. Structural abnormalities: Such as diverticula or surgical alterations. 8. Hormonal imbalances: Affect gut motility and function. 9. Immune deficiencies: Allow overgrowth of harmful microbes. 10. Medications: Such as proton pump inhibitors (PPIs), which reduce stomach acid. What Happens when I eat High FODMAP Foods and Bacteria FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) are short-chain carbohydrates that are poorly absorbed in the small intestine. In SIBO and SIFO, these foods can feed the overgrown bacteria and fungi, leading to fermentation and gas production, which exacerbates symptoms. Treatments for SIBO and SIFO Common Antibiotic Treatments: 1. Rifaximin (not typically covered by insurance, but is the most effective) 2. Metronidazole 3. Neomycin 4. Ciprofloxacin Common Herbal Treatments: 1. Oregano oil 2. Berberine 3. Garlic extract (Allicin) 4. Neem 5. Thyme oil 6. Pau d’Arco 7. Grapefruit seed extract 8. Olive leaf extract 9. Goldenseal 10. Black walnut The FODMAP Diet The FODMAP diet involves restricting high-FODMAP foods and gradually reintroducing them to identify triggers. It helps reduce symptoms by limiting the food supply for harmful bacteria and fungi. Getting Started with FODMAP: • Resources: Monash University’s FODMAP Diet app, “The Complete Low-FODMAP Diet” book by Sue Shepherd and Peter Gibson. (this is the best resource online and the app for creating fodmap diet plan) • Steps: Start with a strict low-FODMAP phase, then reintroduce foods one at a time to determine which ones cause symptoms. Lifestyle Factors Stress, Nutrition, Sleep, and Exercise: • Stress Management: Practice mindfulness, yoga, and relaxation techniques. • Nutrition: Follow a balanced diet that supports gut health, emphasizing whole foods and avoiding processed foods. • Sleep: Aim for 7-9 hours of quality sleep per night. • Exercise: Regular physical activity supports gut motility and overall health. Additional Therapies: • Abdominal Massage: Can help stimulate gut motility. • Castor Oil Packs: Applied to the abdomen to reduce inflammation and support digestion. • Community Support: Engaging with support groups can provide encouragement and shared experiences. Relapse and Triggers Relapse is common with SIBO and SIFO. Common triggers include: • Incomplete treatment- not finishing antibiotics or doing enough rounds of herbs and antibiotics, not long enough in duration. • Poor diet- reintroducing high fodmap foods too soon, not following low for-map diet very well • High stress levels - stress contributes to lower immune function, leaky gut, inflammation and can exacerbate your efforts to heal • Underlying conditions (e.g., IBS )- which is typically associated with anxiety. Impact on Hormones and Quality of Life Hormonal Impact: SIBO and SIFO can disrupt hormonal balance, leading to symptoms like mood swings, fatigue, and menstrual irregularities. Poor gut health can interfere with hormone metabolism and increase inflammation. Quality of Life: Symptoms like constipation, diarrhea, and bloating can significantly impact daily life, causing discomfort, social embarrassment, and emotional distress. In Conclusion: Understanding and managing SIBO and SIFO requires a holistic approach that includes dietary changes, lifestyle modifications, and appropriate treatments. By addressing the root causes and maintaining a supportive environment, you can improve your gut health and overall quality of life. Take care, and remember that managing gut health is a journey, not a destination. :) Yours in health, Dr. Erin Thorne

By Dr Erin Thorne
•
June 23, 2024
Navigating the complexities of Hashimoto’s and hypothyroidism can be challenging, but understanding the condition and embracing a holistic approach can significantly improve your quality of life. Let’s explore what Hashimoto’s is, how it impacts your body, and holistic strategies for managing this condition effectively. What is Hashimoto’s? Hashimoto’s thyroiditis is an autoimmune condition where the immune system mistakenly attacks the thyroid gland, leading to hypothyroidism—a state of underactive thyroid function. The Role of the Thyroid Your thyroid is a small gland located at the base of your neck. It plays a crucial role in: • Hormone Production: Regulates vital hormones like T3 (triiodothyronine) and T4 (thyroxine). • Metabolism: Controls the rate at which your body uses energy. • Weight Management: Influences weight gain or loss. • Skin and Hair Health: Affects skin texture and hair growth. • Mood and Energy Levels: Impacts your mental state and energy. • Temperature Regulation: Helps maintain body temperature. Prevalence and Diagnosis • Prevalence: Hashimoto’s affects millions of women worldwide, making it a leading cause of hypothyroidism. • Diagnosis: Diagnosed through blood tests measuring TSH, T4, T3, and thyroid antibodies. Functional Medicine Lab Order for Hashimotos: • TSH, Free T3 and Free T4, Total T3 and Total T4, Reverse T3, T3 uptake Hormone Production: Regulates vital hormones like T3 (triiodothyronine) and T4 (thyroxine). • Nutrients: iodine, Magnesium RBC, Zinc, CoppuerMetabolism: Controls the rate at which your body uses energy. • Antibodies: TPO, Tg antibodies, TSI, Weight Management: Influences weight gain or loss. • Related infections: Ebstein bar virus (EBV) antibodies, Mycotoxin and mold testing (also another cause of hypothyroid) Skin and Hair Health: Affects skin texture and hair growth. • PCOS markers: insulin, cholesterol, fasting glucose, AST/ALT, HgA1c, Free and Total Testosterone, DHT, DHEA-S, prolactingMood and Energy Levels: Impacts your mental state and energy. • Stool Test: Measures leaky gut, investigates infections contributing to leaky gut or autoimmune, measures microbiome diversity, inflammation, parasites. Temperature Regulation: Helps maintain body temperature. • 4-point Cortisol saliva test: adrenal dysfunction to high or to low impacts thyroid function, and will mimic hypothyroid symptoms. How Hashimoto’s Occurs Hashimoto’s develops through mechanisms like: • Molecular Mimicry: The immune system confuses thyroid cells with foreign invaders. • Leaky Gut: Increased gut permeability allows undigested food particles to enter the bloodstream, triggering an immune response. • Food Sensitivities and Inflammation: Certain foods can exacerbate inflammation. • Genetics: A family history of autoimmune diseases can increase risk. Impact of Chemicals on Thyroid: • Chemicals like Fluoride and Chlorine compete with iodine, disrupting thyroid function. Iodine rich foods may be beneficial in some cases. Avoid prolonged exposure to hot tubs and filter your chlorinated water. Avoid fluoride coating toothpastes is concerned about its impact on your thyroid. Factors Reducing T4 to T3 Conversion: Some women have a normal TSH and T4 on labs with their conventional doctor, however when Free T3 is measured it's low or low-normal, Free T3 is the most bioavaible and active form of thyroid hormone, and not a hormone that you want to be low. T4 converts to T3 in the body and there are a few common culprits of poor conversion of T4 to T3. • Inflammation- due to poor diet, high stress, poor sleep, toxin load is high, elevated antibodies • Infection - leads to increased inflammation, infections most commonly associated with HAshimotos include EBV, mold, SIBO, candida or yeast overgrowth, strep. • Nutrient Deficiencies: " inadequate intake of tyrosine, B6 , B12, iodine, magnesium, selenium, iodine and iron Conventional Treatments Standard treatments include: • Medications: Levothyroxine and Synthroid (T4), liothyronine (T3), and natural desiccated thyroid mixed T3/T4 Naturethrooid and Armour. • Monitoring: Regular blood tests to adjust medication dosages. Holistic Approach to Thyroid Health Nutrition Changes: • Remove Food Sensitivities: Eliminating gluten, dairy, soy, corn, and eggs can reduce inflammation. Night shades are another one that can be a trigger • Whole Foods: Emphasize nutrient-dense, unprocessed foods. • Consider the AIP or Autoimmune Protocol Diet (goggle) 10 Foods High in Thyroid Nutrients: 1. Seaweed: Rich in iodine. 2. Brazil Nuts: High in selenium. 3. Pumpkin Seeds: Good source of zinc. 4. Fish: Rich in omega-3 fatty acids and iodine. 5. Eggs: Contain iodine and selenium. 6. Spinach: High in magnesium. 7. Chicken: Provides tyrosine and selenium. 8. Almonds: Good source of magnesium. 9. Mushrooms: High in selenium. 10. Blueberries: Rich in antioxidants. Key Nutrients and Their Roles: • Iodine: Essential for T3 and T4 production. • B Vitamins: Support energy metabolism and thyroid function. • Selenium: Protects thyroid cells from oxidative damage. • Tyrosine: Amino acid necessary for hormone production. • Magnesium: Supports enzyme function and hormone production. Holistic And Functional Medicine Healing Strategies for Hashimotos: 10 Nutritional Tips: 1. Eat a balanced diet rich in fruits, vegetables, lean proteins, and healthy fats. 2. Avoid processed foods and refined sugars. 3. Incorporate anti-inflammatory foods like turmeric and ginger. 4. Stay hydrated with plenty of water. 5. Limit caffeine and alcohol intake. 6. Eat probiotic-rich foods like yogurt and sauerkraut. 7. Include fiber to support gut health. 8. Consume healthy fats like olive oil and avocados. 9. Opt for organic produce to reduce toxin exposure. 10. Eat regular, balanced meals to maintain blood sugar levels. 10 Ways Stress Impacts Thyroid: 1. Increases cortisol levels 2. Disrupts hormone balance 3. Promotes inflammation 4. Reduces T3 levels 5. Inhibits thyroid hormone conversion 6. Impairs immune function 7. Affects gut health 8. Leads to adrenal fatigue 9. Causes sleep disturbances 10. Triggers autoimmune responses 10 Ways to Manage Stress: 1. Practice mindfulness and meditation. 2. Engage in regular physical activity. 3. Maintain a balanced work-life schedule. 4. Spend time in nature. 5. Connect with loved ones. 6. Pursue hobbies and interests- CREATE something 7. Practice deep breathing exercises. 8. Set realistic goals and prioritize tasks. 9. Seek professional counseling if needed. 10. Establish a relaxing bedtime routine. 5 Ways Poor Sleep Impacts Thyroid: 1. Disrupts hormone production 2. Increases stress hormones 3. Reduces energy levels 4. Impairs immune function 5. Promotes weight gain 10 Ways to Improve Sleep: 1. Maintain a consistent sleep schedule. 2. Create a comfortable sleep environment. 3. Limit screen time before bed. 4. Avoid caffeine and heavy meals in the evening. 5. Practice relaxation techniques. 6. Keep the bedroom dark and cool. 7. Use white noise to block out distractions. 8. Exercise regularly. 9. Avoid napping late in the day. 10. Limit alcohol consumption. 10 Nutrients that Heal the Thyroid: 1. Iodine 2. Selenium 3. Zinc 4. Magnesium 5. Vitamin D 6. Vitamin B12 7. Vitamin E 8. Iron 9. Omega-3 fatty acids 10. Tyrosine Gut Health and the Thyroid Healing the gut and reducing permeability support healthy thyroid function by: • Reducing inflammation • Enhancing nutrient absorption • Supporting immune balance Exercise and Thyroid Function Regular exercise supports thyroid health by: • Boosting metabolism • Reducing stress • Improving mood Examples of Exercises: • Dancing/Walking • Yoga • Strength training • Swimming • Cycling Low Dose Naltrexone (LDN) Treatments for Hashimotos Low Dose Naltrexone (LDN) can support autoimmune conditions by: • Modulating the immune system • Reducing inflammation • Improving overall well-being PCOS and Hashimoto’s PCOS often precedes Hashimoto’s due to shared features like: • Insulin resistance • Hormonal imbalances • Inflammation In Conclusion Managing Hashimoto’s and hypothyroidism holistically involves addressing the root causes, supporting thyroid function through nutrition, lifestyle changes, and stress management. By embracing a comprehensive approach, you can improve your thyroid health and overall quality of life. Yours in health, Dr. Erin Thorne

By Dr. Erin Thorne, ND
•
June 22, 2024
As a naturopathic and functional medicine doctor specializing in women’s health, I cannot stress enough the importance of gut health in maintaining hormonal balance. This blog delves into the intricate relationship between your gut and hormones, particularly focusing on the estrobolome, the gut microbiome, and their roles in managing estrogen levels. Understanding the Estrobolome The estrobolome is a collection of gut bacteria that specifically influence the metabolism of estrogens. These bacteria produce enzymes that help regulate the reactivation and excretion of estrogens, directly impacting their levels in your body. An imbalanced estrobolome can lead to either an excess or deficiency of estrogen, contributing to various health issues. A healthy estrobolome is directly related to women's experience and symptoms in peri/menopause, pcos and endometriosis. Estrogen is a key player in all of those diagnoses and the cleaner the gut microbiome the happier the hormones like estrogen, progesterone, and testosterone. We want the hormones to flow, do their job, then leave in the poop and the urine. We don't want them circulating about in their more toxic forms. I like to think of the hormones living in the ocean or soup of the gut. Women often want to "fix their hormones" or take supplements for their hormones, but truly what you want to heal first is your gut, or you're just wasting your time and money. Otherwise your hormones are trying to communicate and do their job through a sea of inflammation, debris, and toxins. Lets learn how to clean up the gut and why it's important! Imagine trying to get your kids to do their chores with a parade walking in front of them the whole time just wouldn't happen or at least not very well. :) Gut Microbiome and Hormones Your gut microbiome comprises trillions of microorganisms that play a critical role in overall health, including hormone regulation. I tell my patients that YOU are made of 1 trillion cells, but your microbiome is covered in 40-60 trillion microbial cells. Who's really running the show if there are more of them than you? YOU are the CEO of these bugs and we've got to fire some of them, recruit harder workers, and create a healthy work environment otherwise we're going two steps forward 5 steps forward. A healthy gut microbiome helps in the optimal breakdown and absorption of nutrients, supports immune function, and influences the production and regulation of hormones. When your gut health is compromised, it can lead to dysbiosis (an imbalance of gut bacteria), which can negatively impact your hormonal balance. Why We Fix the Gut First, Before Hormones When addressing hormonal imbalances, it’s essential to start with the gut. A healthy gut provides the foundation for balanced hormone levels. Here’s why: 1. Detoxification : A healthy gut efficiently removes excess hormones, preventing their reabsorption. Estrogen goes through the liver and then to the colon for removal in the poop. Many women with imbalanced gut bacteria will reabsorb the estrogen from the colon and pull it back into the body, contributing to excess inflammatory estrogen in the body- the kind that doesn't help with longevity, mood, and all the good things. 2. Inflammation Control: Gut health plays a crucial role in controlling inflammation, which can disrupt hormone production and function. Inflammation can be caused by diets high insular, processed foods, micro plastics and endocrine disrupters (chemicals, pollution in air, water, furniture, new cars). Keeping that ocean we were talking about clean allows for the hormones to communicate more clearly with one another. 3. Nutrient Absorption/Leaky Gut: Proper gut function ensures you absorb essential nutrients needed for hormone synthesis. What if you're just peeing out all your expensive supplements and not even absorbing. There are so many causes of intestinal permeability aka leaky gut. They include: stress, foods you're sensitive too, bacteria byproducts, alcohol and drugs, lack of sleep, high intensity exercise (yep this too!). If your body is busy putting out fires, from bacterial overgrowth, inflammation, infections, toxins its not absorbing nutrients as well as it should, or those nutrients are being utilized to put other the fires instead of "balancing your hormones: like you hoped. Healing Your Gut To restore gut health, consider incorporating the following: 1. Soluble and Insoluble Fiber: Soluble fiber (found in oats, apples, and beans) helps regulate blood sugar levels and feeds beneficial gut bacteria. Insoluble fiber (found in whole grains, nuts, and vegetables) aids in digestive health and regular bowel movements. 2. Prebiotics: Foods like garlic, onions, and bananas act as food for beneficial gut bacteria, promoting their growth and activity. 3. Avoid Sugar and Processed Foods: These promote dysbiosis and inflammation, disrupting gut health and hormone balance. 4. Avoid toxins - foods wrapped in plastics or stored in plastic, unfiltered and bottled water, inorganic foods ( follow the dirty dozen, clean 15 rule), allow new furniture and cars to off gas prior to use. (especially mattresses!) Healthy Estrogen Metabolism Supporting your body’s ability to metabolize estrogen efficiently is crucial. This involves maintaining a healthy liver and gut, as they play pivotal roles in hormone detoxification. Eating a diet rich in cruciferous vegetables (like broccoli and cauliflower) and consuming adequate fiber can enhance estrogen metabolism. Types of Estrogen There are three primary types of estrogen: 1. Estradiol: The most common estrogen in women of reproductive age, most bioavailable and active, low levels associated with hot flashes, infertility, lack of ovulation, dry skin, hot flashes, joint pain and more. 2. Estriol: Predominant during pregnancy. 3. Estrone: The primary estrogen post-menopause. Less potent than estradiol and also has a high propensity to become an inflammatory estrogen in an inflamed gut. Each type of estrogen plays a different role and is metabolized differently, underscoring the need for a well-functioning gut and liver. Gut Health and Women’s Health Issues Improving gut health can significantly impact conditions like PCOS, menopause, and perimenopause: • PCOS: A healthy gut can help manage insulin resistance and inflammation, weight loss and hair loss which are common in PCOS. Hair loss can bel related to hormone imbalances and also nutrient deficiencies and healing your gut should be the first step before taking supplements or medications. • Menopause and Perimenopause: Gut health influences estrogen levels, helping to alleviate symptoms like hot flashes and mood swings. When the estrobolome and microbiome contain overgrowths of yeast, bacteria, mold, and contain larges amounts of micro plastics, endocrine disruptors and inflammatory foods it can make the transition into menopause more challenging. Cleaning up that gut will allow those hormones to communicate to each other more clearly. The Role of Lifestyle Factors- 5 Pillars for Gut-Hormone Health Several lifestyle factors influence your gut microbiome and, consequently, your hormones: #1 Nutrition and Diet: Eating a balanced diet rich in fiber, prebiotics, and whole foods supports a healthy gut microbiome. #2 Exercise: Regular physical activity promotes gut motility and diversity of gut bacteria. #3 Stress Management: Chronic stress can disrupt gut bacteria, so practices like mindfulness and yoga can be beneficial. #4 Toxins: Minimizing exposure to environmental toxins can protect your gut and hormonal health. #5 Sleep: Quality sleep is essential for gut health and hormonal balance. Conclusion By focusing on gut health, you lay the groundwork for balanced hormones and overall well-being. Incorporating fiber, prebiotics, and a healthy lifestyle can significantly improve your gut health, positively impacting conditions like PCOS and menopausal symptoms. Remember, a healthy gut is the cornerstone of hormonal harmony. Take care of your gut, and it will take care of you! Yours in health, Dr. Erin Thorne

By Dr, Erin Thorne
•
October 19, 2023
Perimenopause, the transitional phase before menopause, is a natural and inevitable part of a woman's life. While it can bring about various challenges and changes, adopting a holistic approach to its management can make this transition smoother and more empowering. In this blog post, we will explore the significance of weight-bearing exercise, dietary protein, sleep, stress management, whole foods, and mindfulness as essential elements in managing perimenopause. 1.) Weight-Bearing Exercise Physical activity is a cornerstone of overall well-being, and it plays a crucial role in managing the symptoms of perimenopause. Weight-bearing exercises, such as walking, jogging, or strength training, have several benefits during this phase: a. Bone Health: As estrogen levels decline, women become more susceptible to bone loss. Weight-bearing exercises help maintain bone density and reduce the risk of osteoporosis. b. Weight Management: Perimenopause often brings about weight gain. Regular exercise can help control and even reduce weight by boosting metabolism and muscle mass. c. Mood Enhancement: Exercise triggers the release of endorphins, reducing mood swings, anxiety, and depression – common symptoms during perimenopause. 2.) Dietary Protein Dietary choices are another key aspect of perimenopause management. Protein intake is particularly important for various reasons: a. Hormone Regulation: A balanced intake of protein helps regulate hormones, including insulin and cortisol, which can affect mood and weight gain. Not eating enough protein can contribute to exacerbated symptoms of weight gain, sleep disturbance, moodiness, or fatigue. b. Muscle Preservation: Adequate protein intake supports muscle preservation, which is essential as muscle mass decreases with age. c. Satiety: Protein-rich foods keep you feeling full, reducing the likelihood of unhealthy snacking and overeating. 3.) Sleep Quality sleep is vital for overall health, especially during perimenopause when sleep disturbances are common. Here are some strategies for improving sleep: a. Consistent Sleep Schedule: Maintain a regular sleep schedule to regulate your body's internal clock. b. Create a Relaxing Bedtime Routine: Establish calming activities before bed, such as reading or deep breathing exercises, to reduce stress. c. Limit Stimulants: Avoid caffeine and electronic devices in the hours leading up to bedtime. 4.) Stress Management Chronic stress can exacerbate perimenopausal symptoms. Incorporate stress management techniques into your daily routine: a. Mindfulness Meditation: Mindfulness can reduce stress and enhance emotional well-being. Practice deep breathing and meditation. b. Dance: I'm a huge fan of dance party , mini at home dance party, dance party at the gym or with friends, dance signals to the body that you are safe and open to change and helps allow you to move through sticky emotions and experiences. c. Social Support: Lean on friends and family for emotional support and connection during this phase of life. 5.) Whole Foods Nutrition is an essential component of managing perimenopause. Emphasize whole foods in your diet: a. Fruits and Vegetables: These provide essential vitamins and minerals, as well as antioxidants that combat inflammation. The more colorful your meal the better! Avoid brown and white meals, the color in veggies and fruits indicates all the nutrients you need to feel vibrant! Check out Deanna Minich rainbow Diet. b. Whole Grains: Opt for whole grains like quinoa, oats brown rice, and Ezekiel bread combined with veggies/fiber to stabilize blood sugar levels and provide sustained energy. I know that I require extra carbs and whole grains for energy to dance and keep up with my kids. I recommend carbs prior to an activity but not necessarily before you go sit to work at a computer or watch TV. Make those carbs work! ;) c. Healthy Fats: Include sources of healthy fats, like avocados and nuts, which support brain health and hormone balance. All your hormones are made from cholesterol, avoiding fats can actually harm your hormonal pathways so make sure to include ample healthy fats with each meal. 6.) Mindfulness Lastly, practicing mindfulness can help you stay attuned to your body and emotions during perimenopause: a. Mindful Eating: Pay attention to your body's hunger cues and savor your meals to prevent overeating. As we age and if we are moving our body less and producing less hormones, the truth is that our metabolism slows down, so we really just dont need as many calories as we used to. Being mindful of how much you are eating on a daily basis and what you are eating doesn't have to be a chore but an act of self-care. b. Self-Compassion: Be kind to yourself during this transition and acknowledge that it's a normal phase of life. You are a woman experiencing and completely natural transition in your life. This doesn't have to be the worst chapter o your life, this could actually be the most important or best chapter of your life if you allow for it. I'm a huge fan of journaling "To: Love" a practice I learned from Elizabeth Gilbert on her substack. Letters to love is a daily practice where you write a letter to yourself from the voice of love, often we let the voice of judgment, irritated, or anxious be the dominant voice in our head, strengthening this inner kind voice was a life changing experience for myself and would love for you to learn more about it. Perimenopause is a natural stage in a woman's life that, when approached holistically, can be managed effectively. By incorporating weight-bearing exercise, dietary protein, sleep, stress management, whole foods, and mindfulness into your daily routine, you can navigate this phase with grace and empower yourself to embrace the changes it brings. Remember, every woman's experience is unique, so consult with a healthcare provider for personalized guidance and support during perimenopause.

By Dr. Erin Thorne (Functional and Naturopathic Doctor)
•
October 6, 2023
What are the different types of HRT? There are many options for Hormone replacement therapy. Estrogen is one of the most prescribed hormones for managing menopausal symptoms. 1.) Oral Estrogen: Oral estradiol to manage menopausal symptoms, oral estrogen is associated with higher risks of adverse effects which is why Dr. Thorne prefers topical or transdermal delivery of estrogen. If you have low risk factors, then it is possible the pill would be beneficial for you. 2.) Oral estrogen/Progesterone (BIJUVA): This is bioidentical Estrogen and progesterone delivered in a pill form. Oral estrogens as discussed have higher risks of adverse reactions, but if you have low risk factors then you may be eligible. 3.) Transdermal Estradiol: an estradiol patch applied 1-2 times a week to lower abdomen, back, buttocks , transdermal carries the least amount of risk for adverse reactions. 4.) Oral progesterone: Oral Progesterone is required while on estrogen therapy because a.) Progesterone has been shown to protect uterus while on estrogen therapy. b.) Progesterone complements estrogen therapy and supports sleep and mood among other things. 5.) Vaginal or topical Estriol (E3 form of estrogen): can support vaginal dryness, vaginal integrity, and microbiome support. 6.) Topical Progesterone: although not FDA approved may be utilized to supplement additional progesterone in the body, however it has not been shown to protect the uterus in the same way oral progesterone has. 7.) Topical Testosterone: Testosterone has not been FDA approved for use in menopause. Testosterone is widely used for men later in life to improve muscle mass, libido and energy levels. Women make their testosterone from their ovaries and adrenal glands and levels decline in their 30's. Women may benefit from testosterone in perimenopause to treat energy, libido, and muscle mass. There are some risks associated wit testosterone therapy including clots and liver stress. So best to discus with doctor. 8.) Oral or topical DHEA: DHEA is made from the adrenal glands, and unlike the ovaries in menopause can still create estrogen, progesterone and testosterone. DHEA is kind of like cookie dough in that it has the propensity to make a lot o the necessary hormones in menopause. The issues is that DHEA levels decline with age and chronic stress. DHEA supplementation is not advised without testing first to determine safety and efficacy, since some women may have the genetics to make more toxic estrogens than others with th e"cookie dough." Menopausal women may need to take TWO different types of Estrogen: There are three types of estrogen found circulating in a woman's body. All three types behave differently, and are associated with different levels of risk. Estradiol (E2): Estradiol is the estrogen that is used for treating hot flashes, night sweats among other menopausal symptoms. This type of estrogen is typically administered as a patch or transdermal. (Other doctors may Rx oral versions.) Estriol (E3): Estriol is the estrogen that is used for vaginal dryness and vaginal microbiome and integrity. Estriol (E3) can be inserted vaginally or applied topically. Vaginally inserted estriol can reduce urinary incontinence by supporting structure or vagina, it can provide lubrication for vaginal dryness, and E3 has also been shown to improve vaginal microbiome and reduce infections. Estrone (E1): What is E1/Estrone and Why is it not prescribed? E1 is the most common type of naturally occurring estrogen in a menopausal woman whose ovaries are no longer producing hormones. E1 is derived from fat cells or adipose tissues and from the adrenal gland hormone DHEA. E1 has a higher propensity for contributing to cancers in large amounts so it’s important to monitor levels of E1 in the body with saliva testing and to not Rx any additional E1. Another reason now additional E1 is needed is that Estradiol (E2) can convert into E1 or E3 on its own. Oral estrogen vs Transdermal Estrogen in Menopause: Oral estrogen has a higher risk of causing clots and maybe some cancers than transdermal. Oral estrogens enter the digestive systems, pass through the liver and enter the blood stream. Transdermal or topical estrogens have shown to have lower risk stroke, thrombosis, clots, or cancer. Dr. Thorne prefers using transdermal hormones to mitigate any risk for herself and her patients. Here are some additional considerations: Estradiol pill: oral administration of hormones is common, however more associated with increased risks. If you have low risk factors, then it is possible the pill would be beneficial for you. Estradiol patch: estradiol is administered as a patch on the lower abdomen, buttocks, or belly Estrogen/Progesterone combo pill (BIJUVA) is a bioidentical progesterone and estrogen combined pill designed to treat hot flashes and menopausal symptoms. Resources: 1.) Bioidentical Progesterone safe in menopause, safer than “gestagens” (aka synthetic progesterone) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4245250/ 2.) Oral vs Transdermal Estrogen safety: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10147786/#:~:text=Transdermal%20HRT%20is%20differently%20metabolized,to%20premenopausal%20levels%20%5B10%5D.

By Dr. Erin Thorne
•
October 3, 2023
There are many things to consider when determining your eligibility for HRT. Hormone Replacement Therapy can be beneficial and life changing for many women, however some women it may not be suitable. The research terrain for eligibility is rapidly changing! More research on women's health is emerging, and re-analyzed in the book "Estrogen Matters" that no longer aligns with the standard risk model. There are lifestyle changes and monitoring mechanisms to mitigate those risks, and that'w why working with a functional medicine doctor is optimal in a holistic approach to menopause and HRT. Below you will find 10 things to consider with your doctor for pros/cons/risks/benefits for hormone replacement therapy. Enjoy!

By Dr. Erin Thorne
•
September 29, 2023
Menopause is a natural phase in a woman's life that marks the end of her reproductive years. While it is a significant milestone, it often comes with a range of symptoms that can affect a woman's physical and emotional well-being. Many women turn to Hormone Replacement Therapy (HRT) for relief, but there are also holistic approaches to managing menopause that can be effective, especially when it comes to weight management and alleviating symptoms. Understanding Menopause Menopause typically occurs in a woman's late 40s or early 50s when her ovaries stop producing eggs, leading to a decrease in estrogen and progesterone levels. This hormonal shift triggers a wide range of symptoms, including hot flashes, mood swings, insomnia, and weight gain. The Role of Hormone Replacement Therapy (HRT) Hormone Replacement Therapy (HRT) is a medical treatment that involves replacing the hormones (estrogen, progesterone and sometime testosterone) that decline during menopause. HRT can be effective in reducing or even eliminating many menopausal symptoms. However, it's important to note that HRT is not without risks, and it's not suitable for everyone. It's crucial to discuss the pros and cons with your healthcare provider. Holistic Approaches to Menopause Many women seek alternative and holistic approaches to manage their menopausal symptoms and maintain their overall health. Here are some holistic strategies that can complement or even replace traditional HRT: Diet and Nutrition: Eating a balanced diet rich in whole foods, fruits, vegetables, and lean proteins can help regulate weight during menopause. Foods like soy, flaxseeds, and foods high in calcium and vitamin D can also be beneficial. Exercise: Regular physical activity can help manage weight and reduce the risk of bone loss and muscle atrophy associated with menopause. Aim for a combination of aerobic exercise, strength training, and flexibility exercises. Mind-Body Practices: Practices like yoga, tai chi, and meditation can help reduce stress and improve mood, which can be especially helpful during menopause when mood swings are common. Herbal Supplements: Some women find relief from menopausal symptoms with herbal supplements like black cohosh, evening primrose oil, and red clover. However, it's essential to consult with a healthcare provider before using herbal remedies. Acupuncture: Acupuncture is an ancient practice that involves inserting thin needles into specific points on the body. Some women report reduced hot flashes and improved sleep after acupuncture treatments. Stress Management: High stress levels can exacerbate menopausal symptoms. Engage in stress-reduction techniques such as deep breathing exercises, progressive muscle relaxation, or seeking the support of a therapist or counselor. Managing Weight During Menopause Weight gain is a common concern during menopause due to hormonal changes and a slowing metabolism. Here are some tips for managing weight holistically: Portion Control: Be mindful of portion sizes to prevent overeating. Eating slowly and savoring your meals can help you recognize when you're full. Stay Hydrated: Drinking enough water can help control hunger and prevent mindless snacking. Strength Training: Incorporate strength training exercises into your fitness routine to build muscle, which can boost your metabolism. Sleep: Prioritize quality sleep, as poor sleep patterns can lead to weight gain. Establish a regular sleep schedule and create a relaxing bedtime routine. Mindful Eating: Pay attention to what you eat, and how it makes you feel. Emotional eating can be a common response to menopausal stress. Menopause is a transformative phase in a woman's life, and there are various ways to navigate it holistically. While HRT is an option, it's essential to explore other approaches like diet, exercise, stress management, and alternative therapies to manage symptoms and maintain a healthy weight. Remember that every woman's experience with menopause is unique, so consult with your healthcare provider to determine the best approach for your individual needs and preferences.

By Dr. Erin Thorne
•
April 4, 2023
#1: Adapt to your new bodies metabolism "The ones most adaptable to change will survive and thrive." In menopause your metabolism changes because your entire hormonal system changes. The hormones estrogen and progesterone aren't just involved with having a period and pregnancy, but also your immune system (whether you are allergic to foods or medications), they impact sleep and insomnia, energy levels and mood, and your metabolism. As estrogen and muscle mass decrease with age, this contributes to insulin resistance and abdominal weight gain. (See other blog for more details.) Adapting to your new body and metabolism means that what was working for you before (diet, lifestyle, stress, exercise) may not get you the same results in menopause. I encourage my patients to be open to a new way of eating, exercising, and managing stress, and prioritizing sleep. Menopause is a time to listen deeply to your body, to shed the past and embrace the new. Its also an opportunity to embrace a new way of living and experiencing your life! #2 Change the way you eat: What you ate before menopause may no longer work for you. Take-out food, refined sugars and carbohydrates get lodged much more easily in the fat tissue unfortunately. I like to prescribe my patienst a Libre glucose monitor in menopause so that they can see live time how they're body is responding to different foods. this can help customize their diet. There are 3 things to focus on with meals: 1.) Timing of meals: larger meals should be eaten earlier in the day when metabolism is strongest and smaller meals later in the day. Avoid eating meals close to bedtime. I even recommend early dinners between 5-6. 2.) Portion sizes: with a slower metabolism your portions dont need to be what they once were. You can still enjoy your favorite meals but to support healthy weight make sure your portion sizes fit your new bodies needs. 3.) Avoiding snacks between meals: snacking between meals and snacking after dinner before bed also contribute to weight gain and poor sleep. #3 Change the way you sleep- you eat more calories when sleep deprived! Sleep should really be #1 in all of this because poor sleep can contribute to a perceived 500-600 calorie deficit. Meaning that you want to eat those extra calories to make up for how exhausted your body feels. When we run on low sleep our impulse control is lower and our cravings are more focused on easy energy foods rather than complex healthier foods. You may be used to burning the candle at both ends with a career, kids, taking care of parents but in menopause everything changes and sleep becomes a major priority. Poor sleep also contributes to cortisol imbalance, cortisol by default signals the body to release glucose from the liver and to store more fat because it believes that there is danger with low sleep. If you are having trouble sleeping it could be due to low progesterone, so talk to you doctor about progesterone at bedtime. Circadian Rhythm sleep cycle: our bodies are aligned by our curcadian rhythms, the circadian rhythm determines cortisol, melatonins and hormone levels in the body, and whether we feel energized or sleep. The circadian rhythm is synced with the type of light and darkness we are exposed to. In menopause going to bed early (at least 80% of the time) is essential for healthy hormones and metabolism. Before 10pm, this is non-negotiable and doenst matter if you sleep in. We are light sensitive mammals and our hormones and bodies respond to the rising and setting sun and available light. #4 Change the way you move your body Building and maintaining muscle tone is a must for healthy metabolism in menopause. Muscles are the ticket for becoming more resilient to those "treats or carbs snacks" that you have on occasion. Muscles can soak up sugar without the assistance of insulin. When muscles are weak or reduced then those extra treats are often deposited in the mid-section. Your body will thank you for it because weight lifting and strength training reduces the risk for osteoporosis because exercise imporves bone remodeling, whereas being sedentary or not exercising contributes to bone atrophy/break down. So make weight lifting a part of your menopause journey, Get strong! #5 Changing from Stress Response to Stress Resilience Stress is just part of the human condition, meaning we all have stress during various parts of our lives. Our response to stress is largely a result of our upbringing in childhood to be honest. But with menopause comes the wisdom of experience. You've probably experienced a lot of stress and learned a lot about what matters and what ends up turning out ok. If you haven't then this is something to work on. Your adrenal glands make your stress hormones and in menopause they take over for making your sex hormones. DHEA accompanies cortisol in the body for managing stress, DHEA is the cookie dough that makes estrogen and progesterone iim menopause. So having healthy adrenals and healthy stress responses is essential in menopause. I recommend my patienst all get a 4-point salivary cortisol and DHEA test to assess where they are on the stress spectrum. Form managing stress I recommend letting go of people, situations, environments that are no longer serving you., I recommend working with a therapist on letting go of thoughts and core beliefs that have been haunting you for too long. Menopause is a time for rebuilding the new you, and this requires addressing that which is no longer working for you in your life. How do you want spend the next 50 years?
© 2025
All Rights Reserved | Privacy Policy
Privacy Policy
| Do Not Share My Information
| Conditions of Use
| Notice and Take Down Policy
| Website Accessibility Policy
© 2025
The content on this website is owned by us and our licensors. Do not copy any content (including images) without our consent.



